GLP-1 receptor agonists have moved from diabetes clinics into mainstream conversation. Widely prescribed for type 2 diabetes and increasingly used for weight management, these medications have delivered measurable benefits for blood sugar control and body weight. At the same time, their rapid adoption has raised an important question for patients and clinicians alike: what are the long-term side effects of GLP-1 medications?
- What GLP-1 Medications Are and How They Work
- Why Long-Term Side Effects Matter More Than Short-Term Effects
- Duration of Use and Exposure Considerations
- Gastrointestinal Effects Over Long-Term Use
- Pancreatic Safety and Ongoing Debate
- Gallbladder and Biliary System Effects
- Cardiovascular Effects With Long-Term Use
- Metabolic Adaptation and Weight Plateau Effects
- Muscle Mass and Body Composition Changes
- Hormonal and Endocrine System Effects
- Mental Health and Neuropsychiatric Considerations
- Nutritional Deficiencies With Long-Term Use
- Kidney Function and Hydration
- The Single Most Discussed Long-Term Side Effects
- Differences Between Short-Term and Long-Term Risk Profiles
- Population Differences in Long-Term Risk
- Monitoring and Medical Follow-Up Over Time
- Unknowns and Gaps in Long-Term Research
- Balancing Benefits Against Long-Term Risks
- How Clinicians Approach Long-Term Decision Making
- Lifestyle Factors That Influence Long-Term Outcomes
- Discontinuation and Long-Term Planning
- Public Perception and Media Influence
- Final Thoughts on GLP-1 Long-Term Side Effects
This article examines long-term safety concerns, emerging evidence, biological mechanisms, and unresolved questions surrounding GLP-1 receptor agonists. The focus is not on short-term nausea or early adjustment effects, but on what prolonged use may mean for the body over months and years.
What GLP-1 Medications Are and How They Work
GLP-1 stands for glucagon-like peptide-1, a hormone naturally produced in the gut. It plays a role in regulating blood sugar, appetite, and digestion.
GLP-1 receptor agonists are medications designed to mimic or enhance this hormone’s activity. They bind to GLP-1 receptors throughout the body, including in the pancreas, brain, stomach, and cardiovascular system.
Their main physiological effects include:
-
Stimulating insulin release in response to meals
-
Reducing glucagon secretion
-
Slowing gastric emptying
-
Increasing feelings of fullness
-
Reducing appetite
These effects explain why GLP-1 drugs improve glucose control and support weight loss. They also explain why long-term effects must be evaluated across multiple organ systems.
Why Long-Term Side Effects Matter More Than Short-Term Effects
Most patients experience some short-term side effects when starting GLP-1 therapy, such as nausea or reduced appetite. These effects are well documented and usually improve with time.
Long-term side effects are different. They involve:
-
Changes that persist or worsen over time
-
Effects that appear only after prolonged exposure
-
Physiological adaptations to chronic receptor stimulation
-
Risks that may not surface in early clinical trials
Because many people now remain on GLP-1 medications for years, understanding long-term consequences is essential.
Duration of Use and Exposure Considerations
GLP-1 medications were originally intended for chronic conditions such as diabetes, meaning long-term use was always expected in that population.
However, widespread use for weight management has expanded exposure to younger and otherwise healthy individuals. This shift increases the importance of studying long-term outcomes beyond glucose control.
Long-term exposure raises questions about:
-
Sustained hormonal signaling changes
-
Effects on organ function
-
Metabolic adaptation
-
Nutrient absorption
-
Body composition beyond fat loss
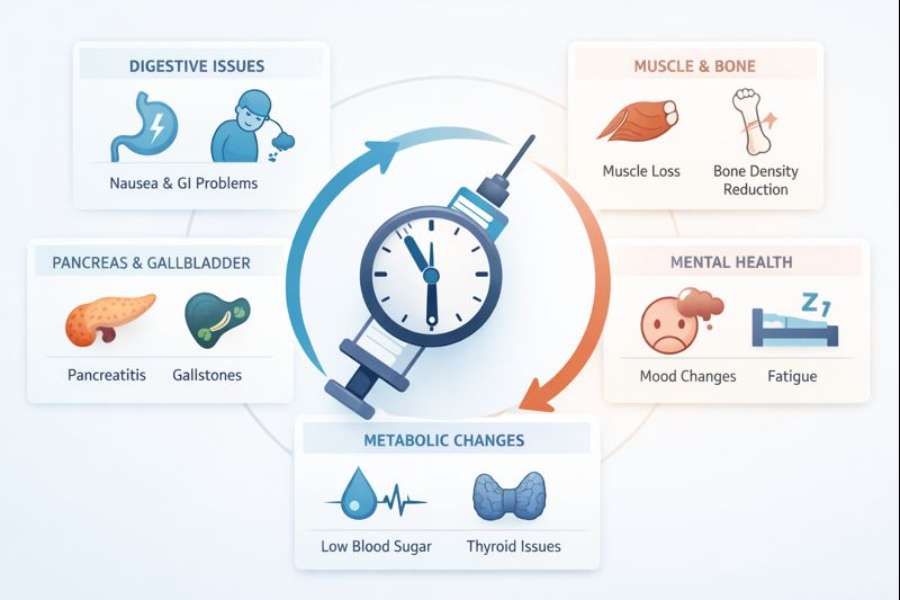
Gastrointestinal Effects Over Long-Term Use
The gastrointestinal system is the most commonly affected by GLP-1 medications, both short-term and long-term.
Persistent delayed gastric emptying
GLP-1 drugs slow stomach emptying. While beneficial for appetite control, long-term slowing may lead to chronic symptoms in some users.
These may include early satiety, bloating, reflux, or discomfort after meals. In a small subset of patients, symptoms persist even after months of therapy.
Risk of gastroparesis-like symptoms
Some individuals develop symptoms resembling gastroparesis, a condition involving impaired stomach motility. Although causation remains under investigation, prolonged gastric slowing may unmask or worsen underlying motility disorders.
Altered bowel habits
Long-term use can lead to chronic constipation or, less commonly, diarrhea. These effects are usually manageable but may affect quality of life.
Pancreatic Safety and Ongoing Debate
Pancreatic effects have been a topic of concern since early GLP-1 development.
Pancreatitis risk
Early post-marketing reports raised concerns about pancreatitis. Large observational studies and clinical trials have not demonstrated a clear causal increase in pancreatitis risk, but vigilance remains.
Patients with a history of pancreatitis are often monitored closely or advised to avoid these medications.
Pancreatic enzyme changes
Some individuals experience mild elevations in pancreatic enzymes without symptoms. The long-term significance of these changes remains unclear.
Gallbladder and Biliary System Effects
Weight loss itself increases the risk of gallstones, regardless of method. GLP-1 medications may indirectly influence gallbladder function.
Gallstones and gallbladder disease
Rapid or significant weight loss can increase bile concentration, promoting gallstone formation. Some long-term users experience gallbladder-related symptoms, including pain or inflammation.
This risk appears related more to weight loss speed than to the medication alone, but GLP-1 therapy may contribute indirectly.
Cardiovascular Effects With Long-Term Use
GLP-1 medications have shown cardiovascular benefits in people with diabetes, but long-term effects still warrant examination.
Blood pressure and heart rate changes
GLP-1 drugs often lower blood pressure modestly. However, they may increase resting heart rate in some individuals. The long-term clinical significance of this increase remains under study.
Cardiovascular outcomes data
Large trials have demonstrated reduced cardiovascular events in high-risk diabetic populations. Whether similar long-term benefits extend to non-diabetic users remains uncertain.
Metabolic Adaptation and Weight Plateau Effects
Weight loss with GLP-1 therapy often slows or plateaus over time.
Adaptive metabolism
As body weight decreases, metabolic rate may adjust downward. This is a normal physiological response but may complicate long-term weight maintenance.
Weight regain after discontinuation
Long-term reliance on appetite suppression raises questions about sustainability. Many individuals regain weight after stopping therapy, suggesting that continued use may be required to maintain benefits. This introduces considerations about indefinite medication exposure.
Muscle Mass and Body Composition Changes
Weight loss is not limited to fat mass.
Lean mass reduction
Some studies suggest that GLP-1-associated weight loss includes loss of lean mass, particularly when protein intake or resistance training is inadequate.
Over long periods, this could affect strength, mobility, and metabolic health, especially in older adults.
Functional implications
Preserving muscle mass becomes increasingly important with long-term use. Monitoring body composition, not just scale weight, is essential.
Hormonal and Endocrine System Effects
GLP-1 receptors exist beyond the pancreas and digestive system.
Appetite regulation pathways
Chronic stimulation of appetite pathways in the brain may alter hunger signaling over time. The long-term impact on natural appetite regulation after discontinuation is not fully understood.
Thyroid considerations
Animal studies raised concerns about thyroid C-cell tumors. Human studies have not confirmed this risk, but individuals with certain thyroid conditions are monitored carefully.
Mental Health and Neuropsychiatric Considerations
Changes in appetite and reward pathways may influence mood and behavior.
Mood changes
Some users report changes in mood, motivation, or emotional response to food. It remains unclear whether these changes are directly caused by GLP-1 medications or secondary to weight loss and lifestyle shifts.
Relationship with food
Long-term appetite suppression can alter eating behaviors and emotional relationships with food. For some, this is beneficial. For others, it may require adjustment or support.
Nutritional Deficiencies With Long-Term Use
Reduced appetite and food intake can lead to nutritional gaps.
Micronutrient intake
Long-term users may consume fewer calories and fewer nutrients overall. Without attention to diet quality, deficiencies in vitamins, minerals, or protein may develop.
Bone health considerations
Reduced intake and weight loss can affect bone density over time, particularly in individuals at risk for osteoporosis.
Kidney Function and Hydration
GLP-1 medications are generally safe for kidney function, but indirect effects exist.
Dehydration risk
Reduced appetite and nausea may decrease fluid intake. Chronic dehydration can strain kidney function, especially in susceptible individuals.
Renal outcomes data
Some evidence suggests potential renal protective effects in diabetic populations, but long-term outcomes in broader populations remain under evaluation.
The Single Most Discussed Long-Term Side Effects
This is the only section where bullet points are used.
-
Persistent gastrointestinal discomfort
-
Gallbladder disease related to weight loss
-
Lean muscle mass reduction
-
Heart rate increases
-
Nutrient intake deficiencies
-
Weight regain after discontinuation
-
Ongoing need for chronic therapy
These concerns are the focus of most long-term safety discussions.
Differences Between Short-Term and Long-Term Risk Profiles
Short-term side effects are usually dose-related and predictable. Long-term risks are more variable and depend on individual factors.
Duration, dosage, baseline health, age, diet, and activity level all influence outcomes. This makes long-term risk assessment more complex than early tolerability.
Population Differences in Long-Term Risk
Not all users experience the same long-term effects.
Older adults
Loss of muscle mass, bone density, and strength is a greater concern in older populations. Long-term use requires careful monitoring.
Individuals without diabetes
Long-term data in non-diabetic populations is still emerging. Risks and benefits may differ from those observed in diabetic trials.
People with pre-existing conditions
Those with gastrointestinal disorders, gallbladder disease, or thyroid issues may face higher long-term risk.
Monitoring and Medical Follow-Up Over Time
Long-term GLP-1 use requires ongoing evaluation.
Clinical monitoring
Regular follow-up allows clinicians to assess symptom persistence, nutritional status, weight trends, and laboratory markers.
Imaging and labs
In some cases, imaging or blood tests help monitor pancreatic, gallbladder, or metabolic changes.
Unknowns and Gaps in Long-Term Research
Despite extensive study, unanswered questions remain.
Duration beyond clinical trials
Many trials span a few years. Effects beyond that timeframe are still being observed.
Lifelong use considerations
As some individuals remain on therapy indefinitely, understanding lifetime exposure becomes increasingly important.
Pediatric and adolescent exposure
Long-term safety data in younger populations is limited and requires careful consideration.
Balancing Benefits Against Long-Term Risks
Long-term side effects must be weighed against benefits.
For many individuals, improved glucose control, reduced cardiovascular risk, and sustained weight loss offer meaningful health advantages. For others, side effects or dependency concerns may outweigh benefits. This balance is personal and evolves over time.
How Clinicians Approach Long-Term Decision Making
Medical professionals consider multiple factors:
-
Individual risk profiles
-
Treatment goals
-
Side effect tolerance
-
Alternative therapies
-
Lifestyle support
Long-term use is rarely a one-size-fits-all decision.
Lifestyle Factors That Influence Long-Term Outcomes
Medication effects do not exist in isolation.
Diet quality
Adequate protein, fiber, and micronutrients reduce many long-term risks.
Physical activity
Resistance training helps preserve muscle mass and metabolic health.
Hydration and supplementation
These support kidney, digestive, and overall function.
Discontinuation and Long-Term Planning
Stopping GLP-1 therapy requires planning.
Gradual transition
Abrupt discontinuation may lead to rebound hunger or weight gain.
Long-term maintenance strategies
Behavioral support, nutrition planning, and activity are critical for sustaining benefits.
Public Perception and Media Influence
Public discussion often focuses on dramatic short-term results. Long-term safety receives less attention but deserves equal focus.
Balanced information helps individuals make informed decisions rather than reacting to hype or fear.
Final Thoughts on GLP-1 Long-Term Side Effects
GLP-1 medications offer powerful benefits, but long-term use brings real considerations. Most long-term side effects relate to gastrointestinal function, body composition, nutritional balance, and the implications of chronic appetite suppression.
Current evidence suggests that GLP-1 drugs are generally safe when appropriately prescribed and monitored. However, long-term outcomes depend on individual health, duration of use, and lifestyle factors.
Understanding potential long-term side effects allows patients and clinicians to use these medications thoughtfully, maximizing benefit while minimizing risk.