Artificial intelligence is no longer an experimental concept in healthcare. It is already embedded in hospitals, clinics, research labs, and insurance systems worldwide. From diagnosing disease earlier to managing patient records more efficiently, AI is changing how care is delivered, measured, and improved. The adoption of AI in healthcare is not about replacing doctors, but about extending human capability in an increasingly complex medical environment.
This article explores how AI is being adopted across healthcare systems, why adoption is accelerating, where resistance still exists, and what the long-term impact will be for patients, professionals, and institutions.
Understanding AI in the Healthcare Context
Artificial intelligence in healthcare refers to the use of algorithms, machine learning models, and data-driven systems to support clinical, operational, and administrative decisions.
Unlike traditional medical software, AI systems learn from large volumes of data. They identify patterns, make predictions, and adapt over time. This ability allows AI to handle tasks that would otherwise require enormous human effort.
Healthcare adoption focuses less on abstract intelligence and more on practical outcomes such as accuracy, efficiency, safety, and cost reduction.
Why AI Adoption in Healthcare Is Accelerating
Healthcare systems worldwide face mounting pressure. Aging populations, staff shortages, rising costs, and increasing data complexity have made traditional models harder to sustain.
AI adoption is accelerating because it addresses these structural challenges.
Healthcare organizations are turning to AI to:
-
Improve diagnostic accuracy
-
Reduce clinician workload
-
Optimize hospital operations
-
Enhance patient outcomes
-
Control long-term costs
These pressures are not temporary. They are systemic, making AI adoption a strategic necessity rather than a trend.
Key Areas Where AI Is Being Adopted in Healthcare
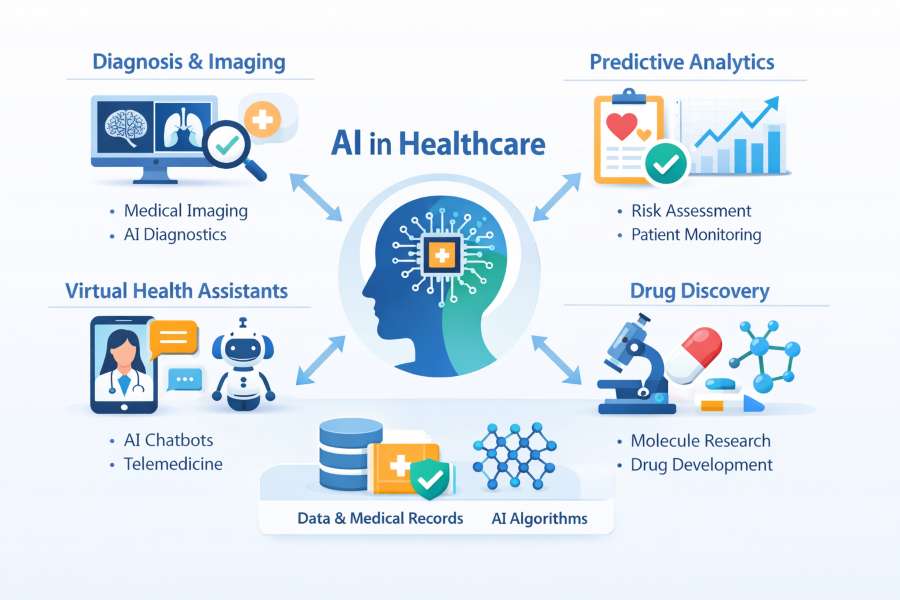
AI is not entering healthcare through a single doorway. Adoption is happening across multiple layers of the system, each with different goals and risks.
Clinical diagnostics and medical imaging
Medical imaging was one of the earliest areas to adopt AI. Radiology, pathology, and cardiology rely heavily on pattern recognition, making them well-suited for machine learning.
AI systems assist clinicians by:
-
Detecting early signs of cancer in scans
-
Identifying abnormalities that the human eye may miss
-
Prioritizing urgent cases
-
Reducing interpretation time
Rather than replacing specialists, AI acts as a second set of eyes, improving consistency and speed.
Predictive analytics and early disease detection
AI models analyze patient histories, lab results, genetic data, and lifestyle factors to predict disease risk.
This capability allows healthcare providers to intervene earlier, often before symptoms become severe. Predictive analytics is increasingly used for chronic disease management, sepsis detection, and hospital readmission prevention.
Early intervention improves outcomes and reduces costs, making this one of the most valuable areas of AI adoption.
Personalized medicine and treatment planning
Traditional medicine often relies on generalized treatment protocols. AI enables more personalized approaches by analyzing how different patients respond to therapies.
In oncology, for example, AI systems help match patients to treatments based on genetic markers and historical outcomes. This reduces trial-and-error prescribing and improves survival rates.
Personalized medicine represents a shift from reactive care to tailored treatment strategies.
AI in Healthcare Operations and Administration
While clinical applications attract the most attention, operational adoption is equally important.
Hospital workflow optimization
Hospitals generate massive amounts of logistical data. AI systems analyze patient flow, staffing levels, and resource utilization to reduce bottlenecks.
These systems help administrators predict peak demand, allocate staff efficiently, and reduce patient wait times. Even minor workflow improvements can lead to significant cost savings and better patient experiences.
Electronic health records and data management
Electronic health records are essential but often burdensome. AI tools are being adopted to automate documentation, extract meaningful insights, and reduce clerical workload.
Natural language processing enables clinicians to dictate notes while AI automatically structures the information. This reduces burnout and allows providers to focus more on patient care.
Revenue cycle and billing automation
Healthcare billing is complex and error-prone. AI helps identify coding errors, detect fraud, and streamline claims processing.
By reducing administrative friction, AI adoption improves financial stability for healthcare organizations without compromising care quality.
The Role of AI in Patient Engagement and Remote Care
Patient-centered care is a growing priority, and AI plays a key role in expanding access and engagement.
Virtual health assistants and chatbots
AI-powered assistants help patients schedule appointments, receive medication reminders, and get symptom guidance. These tools reduce call center volume and improve responsiveness.
When appropriately designed, they enhance access without replacing human interaction.
Remote monitoring and telehealth integration
Wearable devices and home monitoring systems generate continuous data streams. AI analyzes this data to detect anomalies and alert clinicians before conditions worsen.
This approach supports aging populations and patients with chronic conditions, reducing hospital admissions and improving quality of life.
Ethical and Regulatory Challenges in AI Adoption
Despite its benefits, AI adoption in healthcare raises serious ethical and regulatory questions.
Data privacy and security
Healthcare data is highly sensitive. AI systems require large datasets, increasing exposure risk.
Organizations must ensure compliance with privacy laws and implement strong safeguards to prevent misuse or breaches. Trust is essential for adoption to succeed.
Bias and fairness in AI systems
AI systems learn from historical data, which may reflect existing inequalities. If unchecked, this can lead to biased outcomes that disadvantage specific populations.
Healthcare providers must carefully evaluate the model andensure that diverse, representative data is used.
Accountability and clinical responsibility
When AI contributes to a clinical decision, responsibility still lies with human professionals. Clear guidelines are needed to define how AI recommendations should be used and when they should be overridden.
Barriers Slowing the Adoption of AI in Healthcare
Despite strong momentum, adoption is not universal.
Resistance from healthcare professionals
Some clinicians are skeptical of AI systems, particularly when tools lack transparency. Trust develops slowly in environments where errors can have serious consequences.
Education and involvement in system design are key to overcoming resistance.
Integration with legacy systems
Many healthcare organizations rely on outdated infrastructure. Integrating AI with legacy systems is technically challenging and costly.
This slows adoption, particularly in smaller or underfunded institutions.
Cost and return on investment concerns
AI solutions require upfront investment. Organizations must justify costs with measurable outcomes, which can be difficult in complex care environments.
Clear performance metrics are essential for long-term adoption.
The Single Most Important Factors Driving AI Adoption in Healthcare
This is the only section that uses bullet points.
-
Growing demand for efficiency in overstretched healthcare systems
-
Advances in data availability and computing power
-
Shortages of skilled healthcare professionals
-
Pressure to improve patient outcomes and safety
-
Long-term cost containment requirements
These forces continue to push healthcare organizations toward AI adoption despite challenges.
Global Differences in AI Adoption
AI adoption varies significantly across regions.
High-income healthcare systems
Countries with advanced digital infrastructure adopt AI faster, particularly in diagnostics and research. Regulatory clarity and funding support innovation.
Emerging healthcare markets
In developing regions, AI adoption focuses on access and scalability. AI tools help compensate for limited specialist availability and improve rural care delivery.
These systems often leapfrog traditional infrastructure constraints.
AI Adoption and the Future Healthcare Workforce
AI is reshaping roles rather than eliminating them.
Changing skill requirements
Healthcare professionals increasingly need data literacy and familiarity with AI-assisted tools. Training programs are adapting to include these competencies.
Collaboration between humans and machines
AI handles repetitive and data-intensive tasks, allowing clinicians to focus on judgment, empathy, and complex decision-making.
This collaboration enhances care rather than diminishing professional roles.
Long-Term Impact of AI on Healthcare Systems
The long-term impact of AI adoption extends beyond individual tools.
Healthcare systems become more predictive, proactive, and personalized—decision-making shifts from reactive treatment to prevention and early intervention.
Over time, AI adoption may help stabilize costs, reduce disparities, and improve outcomes at scale.
Risks of Overreliance on AI
While AI offers powerful capabilities, overreliance carries risks.
Healthcare decisions involve nuance, ethics, and context that machines cannot fully capture. AI should support, not replace, human judgment.
Balanced adoption ensures technology enhances care without undermining trust or accountability.
Preparing Healthcare Organizations for AI Adoption
Successful adoption requires preparation.
Organizations that succeed tend to:
-
Invest in data quality and governance
-
Train staff early and continuously
-
Pilot systems before large-scale deployment
-
Measure outcomes rigorously
Adoption is a process, not a single implementation.
The Road Ahead for AI in Healthcare
AI adoption in healthcare will continue to expand, but unevenly.
Some applications will mature quickly, while others face regulatory and ethical hurdles. Public trust, transparency, and measurable benefits will determine long-term success.
Healthcare systems that adopt AI thoughtfully will be better positioned to meet future demands.
Final Thoughts on the Adoption of AI in Healthcare
The adoption of AI in healthcare marks a structural shift in how medicine is practiced and managed. It is driven by necessity, enabled by technology, and shaped by human judgment.
AI is not a cure-all, but when implemented responsibly, it enhances efficiency, accuracy, and access to care. The future of healthcare will not be human or artificial. It will be collaborative, data-driven, and increasingly intelligent.